Phagocytosis is one of the first lines of defense against invading microorganisms. It is also important for the processes of tissue remodeling and removal of senescent cells. In the first instance, studies are directed at understanding how living systems defend themselves from foreign bodies and the development of effective therapies against organisms that resist this natural defense system. In the second instance, studies are directed at understanding tissue remodeling during development and repair. While most cells have some capability for phagocytosis, i.e. the need to phagocytose apoptotic cells, the “professional” phagocytes are the phagocytic leukocytes (granulocytes, monocytes and macrophages). Granulocytes are found in the peripheral blood and actively travel to the site of infection by adhering to the vascular endothelium and chemotaxis. Monocytes migrate from the blood stream into the tissues where they differentiate into macrophages. The macrophages extend pseudopods into the lumen of the capillaries to clear the circulation of invading microorganisms.
In general, phagocytosis is initiated by the stimulation of specific receptors on the phagocyte by a ligand on the surface of a particle or invading microorganism. There are three main types of phagocytic receptors: complement receptors, Fc receptors (which recognize the Fc portions of the immunoglobulins), and scavenger receptors (which recognize “non-self” compounds). The complement and Fc receptors recognize the opsonins that are attached to the invading microorganisms by the host, whereas the scavenger receptors recognize microbes directly. Stimulation of the receptors then causes internalization of the particle via an actin-based polymerization mechanism and a phagosome is formed. The phagosome then joins the endocytic pathway to form the mature phagolysosome.
While this general scheme is common to phagocytosis, to date no single model can adequately describe this extremely complex process. This is due in part to the wide variety of receptors that can stimulate phagocytosis and the ability of the microorganisms themselves to influence the process. Added to this is the fact that invading organisms and particles can be recognized by more than one type of receptor and that the receptors can mediate both particle adhesion and internalization. In their review, Aderem and Underhill1 noted that the study of phagocytosis requires an understanding of the mechanisms of signal transduction, actin-based motility, membrane trafficking, and infectious disease.
Synthetic polymeric particles have been used extensively to study phagocytosis. Some of these are styrene-acrylamide copolymer latices5, polyacrolein cellulose, and polyactic / glycolic acid polymers.10, 11 Polystyrene particles are the most often used due to their availability, uniform size, stability, and non-toxic properties. When a small particle that has a narrow coefficient of variation for size is used, as few as one particle per cell can be used and the number of particles ingested per cell can be determined.9,7 Piskin et al.8 conducted studies of phagocytosis by blood cells and mouse peritoneal macrophages using polystyrene microspheres of various sizes and surface properties. Their results illustrate several important points. The first is that the number of microbeads phagocytosed per cell was greatest for the smallest particle they used (0.9µm). Second, the number of particles phagocytosed declined as particle size increased to 6.0µm. Still, both leukocytes and macrophages were able to internalize one or two particles of 4-6µm. Third, the more hydrophobic the particles, the more readily they were phagocytosed. The presences of positively charged amino groups on the less hydrophobic particles increased their uptake. Conversely, the presence of negatively charged carboxyl groups lowered the number of particles internalized. Fourth, coating particles with bovine serum albumin significantly reduced the number of particles internalized whereas coating with fibronectin dramatically increased the phagocytosis of particles.
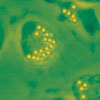
The use of polystyrene microparticles for phagocytosis studies requires that the particles induce the complex series of events involved in phagocytosis. To elicit this response, the particles are first coated with serum (opsonization) or a specific IgG. After opsonization, the particles and the cells are continually mixed at 37˚C during which the phagocytosis occurs. The reaction is then stopped by the addition of ice cold medium and the cells washed to remove any free particles in the medium. The cells are then resuspended in cold medium and analyzed for the number of particles internalized. The quantification of phagocytic activity can be done a number of ways, such as direct microscopic examination, spectrophotometric evaluation, fluorometric evaluation, and flow cytometry. The procedure outlined below gives general guidelines for the preparation of particles and cells and flow cytometric analysis.
Bangs’ polystyrene fluorescent carboxyl microspheres are fluorescent monodisperse polystyrene microspheres that have carboxylate groups on their surfaces. They can be coated passively or the carboxyl groups can be activated for covalent coupling of proteins. Bangs’ fluorescent particles have been used in phagocytosis and neural retrograde transport studies, and as markers for cell bound antigens. These microspheres are packaged as 1% w/v suspension in deionized (DI) water (1mL contains 10mg of fluorescent particles).
Material
Material Required
- Acid citrate dextrose solution-A (ACD-A): 22.0 g/L sodium citrate (Na3C6H5O7H20), 8.0 g/L citric acid and 24.5 g/L dextrose
- Blood sample mixed with the ACD-A anticoagulant (15mL ACD-A / 100mL blood)
- Dextran, pyrogen free (average MW 100,000-200,000 Daltons)
- Ficoll-hypaque lymphocyte separation medium
- Hanks balanced salt solution
- Phosphate buffered saline (PBS)
- Krebs’ Ringers PBS (PBS with 1.0 mM calcium, 1.5 mM magnesium and 5.5 mM glucose [pH 7.3])
- 3.5% NaCl solution
- Sterile water
- 50mL Polypropylene conical centrifuge tubes
- Fluorescent carboxyl particles
- Normal sera or IgG for opsonization
Procedure
Researchers are advised to optimize the use of particles in any application. The following procedure is essentially that reviewed in Harvath and Terle.4 This generalized procedure is intended to be a starting point for the development assays directed at the interest of the investigators and all components of the assay should be optimized to address the specific experimental objectives.
Though beads are processed following synthesis, it is important to note that microsphere suspensions are non-sterile, and may additionally contain residual surfactant, dye, and / or monomer, which could have a negative impact on cells. Microsphere suspensions should be washed prior to use, and suspended in a buffer that is compatible with cells. See also TSD 726, Decontaminating Microspheres, if sterilization / pasteurization is desired.
Cell Isolation
Granulocytes
The following method is according to Boyum2, as modified by Harvath etal.3
- Prepare a solution of 5% dextran in PBS and a 3.5% solution of NaCl.
- Use a fresh blood sample anticoagulated with ACD-A. The blood sample should be maintained at room temperature; do not refrigerate. Perform the cell isolation as soon after the blood collection as possible.
- Add the 5% dextran solution to the blood, 3mL of dextran solution / 10mL of blood. Gently mix and let stand at room temperature for 45 minutes to allow the red cells to sediment.
- Aspirate the plasma layer taking care not to disturb the sedimented red blood cells.
- Isolate the lymphocytes in the plasma by centrifuging through ficoll-hypaque, using a ratio of 2 parts ficoll-hypaque to 3 parts plasma. For this, add the ficoll-hypaque to a conical centrifuge tube and then carefully layer the plasma on to the ficoll-hypaque, such that a sharp interface is visible.
- Centrifuge the tubes at 500 x G for 35 minutes with the centrifuge brake off.
- Carefully remove the platelets and mononuclear cells which are concentrated at the plasma-ficoll-hypaque interface and the rest of the supernatant. Resuspend the pellet containing the granulocytes in 2-3mL of PBS.
- To resuspend the cells, add 24mL of sterile water and gently mix by inversion several times. Add 8mL of 3.5% NaCl and mix gently.
- Add Hank’s balanced salt solution to the mixture to bring the total volume to 50mL. Mix gently and centrifuge at 500 x G for 10 minutes.
- Remove the supernatant and wash the cells 2 times in 20-30mL of Hank’s balanced salt solution.
- Resuspend the cells in 5-10mL of Hank’s balanced salt solution and count. The resuspended cells should contain greater than 98% granulocytes.
Whole Blood
- Fresh blood anticoagulated with ACD-A should be used. The blood should be maintained at room temperature and the assay performed within 5 hours of collection.
- In general, plan on using 100-200µL of whole blood per assay.
Note: Microspheres should be washed before opsonization or use in the phagocytosis assay to remove surfactants and other additives.
Opsonization
- For opsonization with normal serum, add particles to serum that has been diluted to 50% with Krebs’ Ringers PBS. Gently mix and let incubate for 30 minutes at 37˚C. After incubation, the particles are added to the phagocytosis assay mixture at concentration equivalent to ~5% serum. Adjust the particle density to 108 particles/mL.
- For optimization with a specific immunoglobulin, it is important to determine the concentration of immunoglobulin that does not cause aggregation of the particles. The immunoglobulin is incubated with the particles for 60 minutes at 37˚C. Following the incubation, the particles are washed 3 times with PBS and the particle density adjusted to 108 particles/mL.
Phagocytosis Assay
Isolated Cells
- Add 100µL of granulocytes (107 cells/mL in Krebs’ Ringers PBS) to a polypropylene tube.
- Add 10µL of the opsonized particles (108 particles/mL) to the tube and incubate with gentle shaking for 30 minutes at 37˚C.
- As a control, prepare an identical sample that is incubated at 4˚C.
- At the end of the 30 minute incubation, stop the phagocytosis by adding 2mL of ice cold PBS. Mix and then wash the cells 2 times with ice cold PBS.
- Resuspend the cells in 500µL of cold PBS, keep the samples at 4˚C and analyze as soon as possible.
Whole Blood
- Add 200µL of anticoagulated whole blood to a polypropylene tube.
- Add 10µL of the opsonized particles (108 particles/mL) to the tube and incubate with gentle shaking for 30 minutes at 37˚C.
- As a control, prepare an identical sample that is incubated at 4˚C.
- At the end of the 30 minute incubation, stop the phagocytosis by adding 2mL of ice cold PBS mix and then wash the cells 1 time with ice cold PBS.
- Resuspend the cells in 3mL of sterile water and gently mix for 20-30 seconds. Add 1mL of the 3.5% NaCl to make the suspension isotonic and pellet the cells by centrifuging at 500 x G for 5 minutes.
- Resuspend the cells in 500µL of cold PBS, keep the samples at 4˚C and analyze as soon as possible.
Flow Cytometric Analysis
- Adjust the forward and right-angle scatter detectors so that the granulocyte population is clearly visible and gate on the granulocyte population for analysis.
- The experimental sample is analyzed by setting the appropriate fluorescence detectors so that several distinct population peaks are easily distinguished. The different peaks should correspond to cells that do not contain particles and those that have internalized 1, 2, 3, or more particles.
- Once the optimal fluorescence gain settings have been established, analyze 10,000 cells. Adjust the forward and right-angle scatter detectors so that the granulocyte population is clearly visible and gate on the granulocyte population for analysis.
References
1. Aderem, A., D.M. Underhill. 1999. Annu Rev Immunol, 17:593-623.
2. Boyum, A. 1968. Scand J Clin Lab Invest, 21(Suppl. 97):77-89.
3. Harvath, L, J.A. Balke, N.P. Christiansen, A.A. Russell, K.M. Skubitz. 1991. J Immunol, 146(3):949-957.
4. Harvath, L, D.A. Terle. 1999. Meths Mol Biol, 115:281-290.
5. Kawaguchi, H., N. Koiwai, Y. Ohtuska, M. Miyamoto, S. Sasakawa. 1988. Biomaterials, 7(1):61-66.
6 Kawaguchi, H., H. Hoshino, H. Amagasa, Y. Ohtsuka. 1984. J Colloid Interface Sci, 97(2):465-475.
7. Parod, R.J., J.D. Brain. 1983. Am J Physiol, 245(3):C227-234.
8. Piskin, E., A. Tuncel, A. Denizli, H. Ayhan. 1994. J Biomater Sci, 5(5):451-471.
9. Steinkamp, J.A., J.S. Wilson, G.C. Saunders, C.C. Steward. 1982. Science, 215(4258):64-66.
10. Tabata, Y., Y. Ikada. 1988. Biomaterials, 9(4):356-362.
11. Tabata, Y., Y. Ikada. 1991. Phagocytosis of Polymeric Microspheres. In: High performance biomaterials, M. Szycher, ed.. Lancaster, PA:Technomic Publishing Group.
Click for additional phagocytosis references
